Sperm is produced in the testes in response to stimulation by a brain gland called the pituitary. The sperm is then stored and matures in the “tail” of the testes at the epididymis. Sperm then travels through a long narrow tube called the vas deferens and is released during ejaculation by way of an ejaculatory duct which travels through the prostate and releases the sperm into the urethra which travels through the penis. The actual ejaculate contains sperm plus prostatic fluids plus fluid from the seminal vesicles.
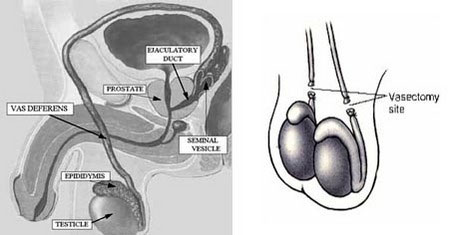
Vasectomy, or “male sterilization,” is a procedure where the vas deferens is surgically blocked by tying and cutting it. Thus the sperm cannot escape from the testes. Vasectomy is intended to be a permanent form of sterilization, much like a tubal ligation for the female.
How is vasectomy reversal performed? There are basically two options: surgical or nonsurgical.

The nonsurgical option involves an office biopsy of the testes. This is done under local anesthesia. A small piece of the testes is “snipped”. It is then examined for the presence of sperm and then rapidly frozen. This process is referred to as testicular aspiration (TESA) or testicular extraction (TESE). The wife then undergoes another nonsurgical procedure called in vitro fertilization (IVF).
This process involves stimulation of the ovaries with medication. The eggs are then harvested by a nonsurgical ultrasound technique. Each mature egg is then injected with sperm (ICSI). Two or three embryos are then transferred into the uterus through the cervix. Two weeks later, a pregnancy test is performed. Pregnancy rates for in vitro are about 50% for younger women ( 35 and under ). Extra embryos can be frozen and used later at lower cost to achieve pregnancy.
The nonsurgical technique can be performed after any type of vasectomy. The odds of success are not influenced by the number of years since vasectomy. The odds of success with surgical reversal decline after the vasectomy has been in place for 5 years. Young women can achieve a pregnancy rate of 50% in one IVF cycle which takes 2 months to complete compared to an average of 12 months to conceive after surgical vasectomy reversal.
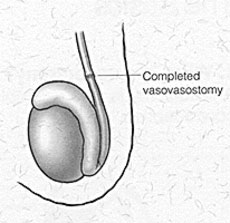
In many cases it is possible to reverse the vasectomy. If the original procedure was not too damaging and it has not been too many years, it is possible to reconnect the vas deferens on one or both sides. This procedure involves a general anesthetic. An incision is made in the front of each side of the the scrotum and under a microscope the vas is reconnected. Operating time is 2 to 3 hours in the average case. During the procedure they check to make sure the side close to the tests contains sperm. If it does not they mayhave to connect the distant portion to the epididymis. This does not give as good a pregnancy rate.
Slight swelling, bruising, or discoloration of the scrotum is common after surgery. Ice packs and pain medication are typically required after the surgery. It is generally best to abstain from intercourse for 3 weeks following the procedure. Sperm will reappear in the ejaculate 4 to 6 months after reversal. Peak sperm counts may take 12 to 24 months to appear. Sometimes the sperm count will peak and then begin to decline due to scar tissue formation.
The chance of pregnancy after reversal depends on many factors. The time between vasectomy and reversal is one important factor. If the procedure was done between 3 and 8 years ago a pregnancy rate of about 50% can be achieved within 18 months. After 9 to 14 years the pregnancy rate is about 44%. The average time between vasectomy reversal and pregnancy is 12 months.
The first is the obvious. One is with incisions and a general anesthetic. The other does not involve surgery. If vasectomy reversal was more than 5 years ago, nonsurgical IVF may be better. IVF is more prone to multiple births because typically 2 embryos are transferred. About 25 – 30% of births with this technique are twins whereas surgical repair is not associated with any increase in the multiple birth rate. The average time to conception is shorter with IVF compared to surgical repair. If you have surgical repair you may need another vasectomy later. With nonsurgical since the vasectomy is left in place, you will not need another vasectomy.
The ideal choice for you depends on your particular situation. Feel free to discuss both options with a reproductive endocrinologist, obstetrician or urologist.