Approximately 15-20% of couples attempting to achieve pregnancy in the United States each year face difficulties with fertility. Of those couples, a pure “female factor” is responsible for about 35-40% of cases. About another 35% of cases are pure “male factor.” Couples with a combination of male and female factors account for the remaining 25-30% of cases. Therefore, a male infertility factor plays a part for more than 50% of couples unable to conceive on their own. These numbers stress the need for appropriate male factor evaluation and treatment options.
Many different factors can affect male fertility. Sexual function is the most obvious of these factors, and sexual dysfunction (or the inability to ejaculate sperm into the vagina of the female partner) accounts for a small but significant portion of male factor cases. Many kinds of lubricants frequently used as aids for intercourse can kill or slow sperm down. Too lengthy intervals between episodes of ejaculation can also cause reductions in sperm motility.
Many prescription drugs can interfere with the production or function of sperm. Some antibiotics, blood pressure medications, ulcer medicines, and steroids are potential causes for sperm dysfunction. In addition, drugs of abuse like alcohol, cocaine, marijuana, and even tobacco can have deleterious effects on sperm.
A recent common problem has been testosterone therapy for men with “low Testosterone”. It is not widely known even by doctors that small amounts of testosterone will cause a drop in sperm counts. If you are on Testosterone please inform us and your treating physician. It is possible to give medication such as clomid to increase your body’s production of testosterone without dropping the sperm count.
Finally, physical illnesses such as diabetes and hypertension can have effects on spermatogenesis. Structural problems like a varicocele or congenital absence of the vas deferens may cause sperm problems. Your physician may recommend you to a specialist like a reproductive urologist for the evaluation of these conditions. Occasionally hernia repairs or other groin surgery can lead to male factor fertility concerns. Finally genetic considerations (like cystic fibrosis, or small deletions or rearrangements of the genetic material on the Y chromosome) are frequently associated with severe male factor infertility. Testing is available for many of these considerations and may be recommended by your physician.
The semen analysis is the standard for evaluating semen parameters. Private and comfortable collection facilities are available at the laboratory of the Institute for Reproductive Health. If patients live nearby the facility, arrangements can often be made for a semen collection at home to be brought into the lab by the couple. Your physician will typically recommend 2-5 days of abstinence prior to the collection in order to accurately assess the sperm parameters. A sample is usually collected by masturbation into a sterile container provided by the laboratory.
The semen analysis is usually divided into several parts. The ejaculate volume is assessed. Many people are surprised to learn that a normal ejaculate volume is only around ½-1 teaspoon. The sperm count is extremely important and is reported as a concentration in millions of sperm/mL. Normal values are usually considered >20M/mL. Motility, or the percentage of sperm that are swimming or moving, is another important parameter to evaluate. Typically, it is healthy to have 50% or more of the present sperm swimming. Progression, or how well the sperm are able to move forward in a straight direction, is also assessed or graded (usually on a scale of 0-4). The semen is also analyzed for the presence of white blood cells that may indicate an infection (often in the prostate gland). In cases where sperm is absent all together (azoospermia), analysis of the ejaculate fluid may reveal the presence of a mechanical blockage in the sperm outflow tract.
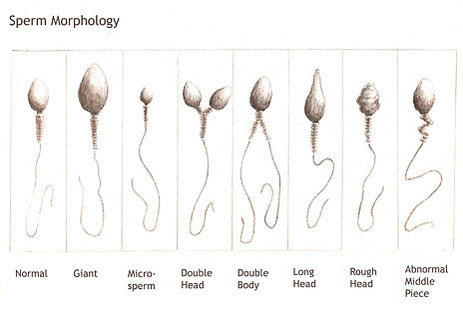
Perhaps one of the most important factors looked at in the semen analysis is the Kruger’s Strict Morphology. This is a microscopic examination of specially stained sperm that details the shape of the sperm, evaluates the normalcy of the sperm heads and tailpieces, and their relationship to one another. Most laboratories in the hospital setting are not able to provide this kind of analysis. It should be done at a reproductive center. Experience with the assisted reproductive technologies like in vitro fertilization (IVF) has allowed us to take the index achieved from a morphology analysis and help predict how likely a sperm is to be able to bind, penetrate, and fertilize an egg even if placed in close proximity to that egg. This gives us a good clue as to sperm function. In our laboratory, 4% or more completely normal sperm correlates with good fertility potential.
There are other measures of sperm viability and function like the postcoital test, the sperm penetration assay, the osmotic swelling test, or the hemizona binding assay, but these tests are becoming less clinically relevant as the advanced reproductive technologies have vastly improved in the last decade.
The number of options for the treatment of male factor fertility has grown dramatically over the last 10 years. Lifestyle changes and removal of inciting medications can be an important step in the right direction. Timing and frequency of intercourse can often be improved. Intrauterine insemination (IUI, formerly known as artificial insemination) is a process whereby washed sperm from the husband is placed using a tiny flexible tube right at the opening of the fallopian tubes in the wife’s uterus to get more sperm closer to where they need to be effective. IUI will also help overcome cervical factor infertility (abnormal cervical mucus or antibodies against the sperm that can kill sperm). IUI is a relatively inexpensive procedure, and most women describe the experience as similar to having a Pap smear done. For more information on IUI follow the link to Basic Therapy. The following is a diagram showing the insemination procedure which is done in the office setting much like a pap smear.
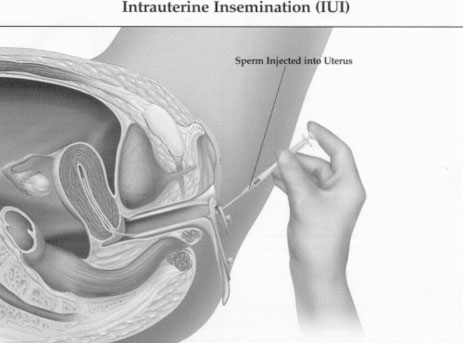
Intrauterine Insemination (IUI)
The advent of ICSI (intracytoplasmic sperm injection) as an adjunctive therapy to IVF has led to the successful birth of thousands of babies born to men who previously had no fertility options and no chance of having their own biologic children. With ICSI, a single sperm is taken and injected directly into an egg under a high power microscope. With this process, even sperm that is unable to bind or penetrate an egg can still be used to fertilize an egg and create an embryo to be implanted in a woman’s uterus. Sometimes sperm can even be retrieved from the testicles of men with no sperm in their ejaculate and used for ICSI with great success.
Intracytoplasmic Sperm Injection
For more information about IVF and ICSI please follow the link to the In Vitro section of the web site.
Finally, for many couples with a severe male factor, therapeutic donor insemination represents a wonderful chance for parenting. With this process, the couple chooses an acceptable and carefully screened and tested donor from a reputable sperm bank, and a frozen sample of sperm is thawed an placed in the woman’s uterus with IUI (as described above). This is done at the point in the woman’s cycle to coincide with the release of her egg (ovulation).
Male factor infertility is an important contributor in half of all couples who are having trouble conceiving. No fertility evaluation is complete without a careful semen analysis, even for men who have had children in the past. Many inexpensive and simple treatment options are available to help couples with male factor infertility conceive. The advent of ICSI has allowed us to achieve fertilization in most of our extremely severe male factor cases. A careful discussion of these matters with your physician can help choose the workup and treatment plan that best suits your needs.