Many patients with infertility may also suffer from one or more miscarriages. A miscarriage is a true loss for a couple, and its emotional and physical impact should not to be underestimated, especially in couples who may have been trying for years to get pregnant.
A miscarriage occurs when a pregnancy is lost less than 20 weeks from the last menstrual period. Losses after this time period are considered births, even if the baby is not born alive or dies soon after delivery. Miscarriages are extremely common. About 20 percent of all pregnancies will end in a clinical miscarriage. That doesn’t even include all the early losses which we call biochemical pregnancies that occur before a pregnancy sac forms in the uterus. These biochemical pregnancies are typically recognized as a delayed menstrual period in women with normal cycles where the pregnancy test is slightly positive for a few days followed by spontaneous menstruation.
A true miscarriage typically will occur between 6 and 20 weeks of pregnancy. For a miscarriage to occur, a clinical pregnancy must first be established. A clinical pregnancy is one in which an examination reveals an enlarged uterus or a pregnancy sac is seen in the uterus by ultrasound. These definitions may seem a bit narrow, but it is important to understand that biochemical pregnancies are even more common than miscarriages. It is estimated that as many as 60 percent of all early identified pregnancies end in biochemical losses. Biochemical pregnancies are not abnormal. For that matter miscarriage is not abnormal. Both are nature’s way of not letting an abnormal pregnancy continue to result in an abnormal birth. Both processes can be nature’s way of increasing your chance of having a healthy baby.
If you have ever had a miscarriage, you have undoubtedly wondered why it happened. Was it something you did or didn’t do? Was it a medication you took? Does it have anything to do with level of activity? Most miscarriages are completely beyond the control of the couple or their physician, and they occur spontaneously because of chromosomal or genetic problems existing within a particular fetus. An embryo or fetus with the wrong number of chromosomes is called aneuploidic. The most common aneuploidies involve either an extra chromosome that may not be compatible with life or a missing chromosome that is necessary for life. Some kinds of aneuploidy can still result in a live birth (examples are Turner’s syndrome or Down syndrome), but many result in miscarriage. The vast majority of losses in which a fetus without a heart beat is seen on ultrasound are due to chromosomal errors.
The chance of a chromosomal error and miscarriage increases dramatically with the age of the mother. While the risk of miscarriage in the general population is about 20 percent, in women 40 or more years of age it is a staggering 40-50 percent! That is why we want you to try to get pregnant while you are younger, so you do not have to face these tough odds.
In addition to the age of the mother, other poorly controlled medical conditions such as diabetes, high blood pressure and asthma can increase the risk of miscarriage. Abnormalities or scarring of the uterus and cervix may pose anatomic risks for recurrent miscarriage. Also, if you or your partner carries a genetic abnormality such as a translocation (one piece of genetic material is an abnormal place), your risk is increased. Smoking, drinking and use of recreational drugs such as marijuana or cocaine can also increase the risk of loss. Caffeine can increase the risk of miscarriage. Most studies show that more than 200 milligrams per day needs to be consumed to significantly increase the risk of miscarriage. Some studies have shown a slight increase in risk with lesser quantities. A serving of coffee, tea, or a caffeinated soft drink can contain up to 100 milligrams of caffeine. A common sense measure is therefore to limit yourself to one or two caffeinated beverages per day. Rarely an infection can cause a miscarriage. Examples of infections associated with miscarriage include viral infections such as cytomegalovirus (CMV), rubella and measles. Sometimes bacterial infections such as Streptococcus or gonorrhea can cause a pregnancy loss.
Certain medications taken during the first trimester may also increase miscarriage risks. These include chemotherapy and some anti-seizure drugs. Chemical substances in the environment can also cause miscarriage. Some examples are lead, which is found in car batteries, and formaldehyde, arsenic and radiation. Age of the father is also a risk factor, although to a much lesser extent than age of the mother. If you have had two or more consecutive miscarriages, your risk of miscarriage is also increased, and you may want to seek help from a reproductive endocrinologist before trying to conceive again.
Heavy bleeding and uterine cramping are the most common signs of an impending miscarriage. Bear in mind, though, that light bleeding or spotting coupled with mild uterine cramps are very common in early pregnancy and usually do not progress to miscarriage. Less commonly, bleeding and cramping in early pregnancy can be a sign of tubal or ectopic pregnancy. With ectopic pregnancy the pain is often on one side of the abdomen and is more severe.
It is usually not possible to know immediately what type of pregnancy is occurring in the face of cramping and bleeding. Blood tests can diagnose pregnancy at the time of missed menses. Two weeks later an ultrasound can see an early six-week pregnancy in the uterus. The risk of miscarriage will drop after we see the fetal heart beat on ultrasound. This is usually seen six to eight weeks after the last menstrual period. If you think you are miscarrying, call your doctor. In most cases he or she will see you as soon as is feasible and perform an exam and an ultrasound and possibly blood tests to evaluate your situation. If you show signs of miscarriage your doctor may ask you to reduce activity, although it is not clear that this will reduce your chance of losing the pregnancy. Most practitioners will also ask you to abstain from intercourse during this time. Tylenol is the most commonly prescribed medication to treat the cramping pain.
There are basically three treatment options for women who have been diagnosed with a nonviable pregnancy in the uterus but have not passed the fetal tissue yet. The first option is expectant management. In other words, we do nothing and wait one or two weeks to see if your body naturally expels the tissue. If more than two weeks go by without bleeding, then some other treatment may be warranted.
Some women elect to have medical therapy. Hormones that are often used to induce labor in women who go past their due date can also be used to help induce the body to expel the fetal tissue once we are positive that the pregnancy is not progressing. These tablets are usually taken vaginally and can be very effective within one or two days of initiating treatment. After either a natural or an induced miscarriage, a physician should examine you to make sure the uterus is completely emptied.
The potential advantages to either of these first two options are that there are no surgical procedures involved and the process is relatively natural. The significant disadvantages include moderate to severe pain and bleeding which can turn into an emergency situation, as well as the unpredictable nature of when a miscarriage may occur. It can be especially hard for women with a history of infertility to walk around for weeks with a pregnancy they know is no longer viable waiting for cramping and bleeding to start.
Finally, some women will opt to have a D&C (dilatation and curettage). This is a minor surgical procedure in which the cervix is gently dilated and the uterus is emptied using a suction instrument. This is often done under general anesthesia, but can also be performed with mild sedation and a local anesthetic block placed in the cervix. The advantage of the D&C is that it spares the patient the pain of heavy bleeding and cramping associated with a natural miscarriage. A D&C can also be scheduled so that the event occurs at a predictable time. Disadvantages to the D&C include the minor risks of anesthesia or surgical complications such as injuring or scarring the uterus. These complications probably occur in less than 1-2 percent of cases.
After any type of miscarriage or ectopic pregnancy, you may need a shot of Rhogam if your blood type is “Rh negative” (e.g. O negative, A negative, etc.). This shot will help prevent complications in future pregnancies related to potential incompatibilities in blood types between partners. Following a D&C or natural miscarriage, you can expect your menstrual period to restart within six weeks if you had regular periods prior to conception. Your menstrual cycles will then resume their normal pattern.
When can you try to get pregnant again? The length of time you should wait before trying to conceive again may depend on the type of miscarriage, how it was treated, or if there were any complications. Most couples, however, can resume their conception efforts after one to three cycles. You should discuss this with your doctor, as it will vary from case to case.
The answer in most cases is no! Miscarriage is a common part of human reproduction. That is not to say that experiencing a miscarriage is easy. It is miserable, depressing experience. The good news after a miscarriage, however, is that you did manage to conceive. This usually means that the reproductive system is working to a certain degree. If you have had two or three consecutive pregnancy losses, then your risk of future miscarriage may be increased, and a workup should be contemplated. Even if you have had three consecutive miscarriages, your chances of a future live birth are still almost 70 percent. The glass is definitely more than half full!
If you have experienced more than two or three consecutive pregnancy losses, your physician may recommend doing an evaluation to identify certain treatable risk factors. A study of the internal structure of the uterus should be performed, either through an x-ray of the uterus (hysterosalpingogram or HSG) or a sonohysterogram, which is an ultrasound done after instilling fluid into the uterine cavity. In some cases there is a deformity in the uterus, such as a wall or septum inside the uterus or a double uterus.
Some deformities of the uterus are imaged below:
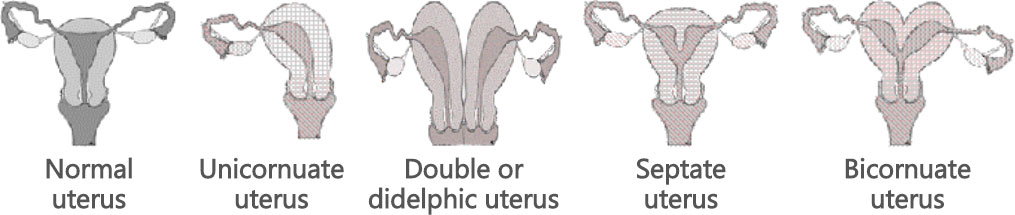
If there is a septum or scarring in the uterus, then surgery performed as an outpatient (hysteroscopic surgery) can be used to correct this. The greatest benefit in repair is with the septate uterus. Studies in patients with a septate uterus have shown that, before surgery about 70 percent of all pregnancies are miscarried while after surgery only 30 percent are lost to miscarriage. It is not possible to enlarge the unicornuate uterus, and a didelphic uterus can rarely be repaired.
In addition to examining the structure of the uterus, your doctor will likely order some blood tests. Checking the chromosomes (the genetic structure of the cells) and the chromosomes of the male and female can be helpful. In some cases, one member of the couple may have a piece of one chromosome that has shifted to another area of the gene structure. This is called a translocation and can increase your risk for miscarriage. If you have this condition, it is possible to do in vitro fertilization and test the embryo’s genetic make-up by a process called preimplantation genetic screening (PGS).
Other common testing may screen for blood clotting problems in the female partner. Blood clots that form in the bed of the placenta can cause pregnancy loss, especially after 12 weeks. Testing for blood clotting disorders is complex, but some of the more common tests look for lupus anticoagulant, anticardiolipin antibody, Factor V Leiden, MTHFR gene mutations, and the prothrombin gene mutation. If you have a clotting disorder you may need anticoagulation treatment (or blood thinners) during pregnancy. This is in the form of heparin, aspirin or other medications. Anticoagulation should be used only when there is a clear need because it carries with it an increased risk of bleeding.
Endocrine testing is also part of the evaluation of recurrent pregnancy loss. You may be screened for thyroid disease, diabetes, or high prolactin levels. Your workup may also include testing for autoimmune processes. Fortunately, except for the uterine testing, most of the workup simply involves blood work. For couples experiencing multiple losses, genetic or chromosomal testing of the fetal tissue may also be revealing. This is usually best accomplished at the time of a D&C.
In most cases, a specific cause of the miscarriage is not identified. Many women in this case may elect to take a baby aspirin that may help reduce inflammation or blood clotting tendencies. But take heart, even after repetitive miscarriages, many couples are still able to deliver healthy babies.
A miscarriage is bad enough normally, but after infertility treatment it seems unusually cruel. It just doesn’t seem fair to have to go through a miscarriage after struggling with infertility! It seems as though if it weren’t for bad luck, you’d have no luck at all. Remember that it is normal to feel sad. Miscarriage is a real loss. Try to ignore the comments of others who don’t understand. It hurts to hear them say: “Don’t worry, you’ll get pregnant again,” when you struggled so hard to get pregnant. Give yourself some time to grieve. Time does heal some wounds. Try to understand that it is a loss for your partner, too. He or she is going through his or her pain, also. Your partner may not always say the right thing. When you’re up to it, talk to your doctor about restarting fertility treatment. Remember that a miscarriage means conception is possible, and the odds are in your favor for a healthy outcome with a subsequent pregnancy.
Unfortunately, miscarriage is an all-too-common problem. However, an appropriate workup and evaluation can help reduce the chance of a subsequent loss.